Recently the BBC has reported that around a million people in the UK have type 2 diabetes, but are unaware of it, putting their lives at considerable risk.
What’s more concerning is that the prevalence of diabetes is rising rapidly in younger age groups, and diabetes is more likely to go undiagnosed if you’re younger.
The Office for National Statistics has shown that half of people who are aged 16 to 44 who are screened for diabetes and are found to have type 2 diabetes have gone undiagnosed.
What’s also interesting is that type 2 diabetes is more likely to be undiagnosed when a person appears to be in good health, and in women who aren’t overtly overweight.
There is a stage before the development of ‘full-blown’ type 2 diabetes which is known as pre-diabetes. This is when a person’s blood sugar levels are higher than normal but not yet high enough for a diagnosis of type 2 diabetes.
Not everyone who develops pre-diabetes is overweight or obese, and around 1 in 20 people aged 16 -44 who have pre-diabetes are of normal or even low weight.
Am I at risk of developing diabetes or pre-diabetes?
You’re more likely to develop diabetes or pre-diabetes if you’re of Asian or Black ethnicity, or if a parent or sibling has type 2 diabetes.
Being overweight (i.e. having a BMI greater than 25), excessive body fat, and being physically inactive also increases your risk, as does eating highly processed foods.
Some medical conditions such as hypothyroidism, Cushing’s disease, polycystic ovary syndrome, and having had gestational diabetes, can predispose you to pre-diabetes, as can taking long-term steroid medications for inflammatory conditions.
We also know that poor quality sleep, too little sleep, or difficulty getting off to sleep are risk factors for pre-diabetes. Obstructive sleep apnoea also increases your risk.
Smoking increases your risk of pre-diabetes because it makes your cells more resistant to insulin, and people who smoke are 30-40% more likely to develop type 2 diabetes.
What is happening metabolically in pre-diabetes?
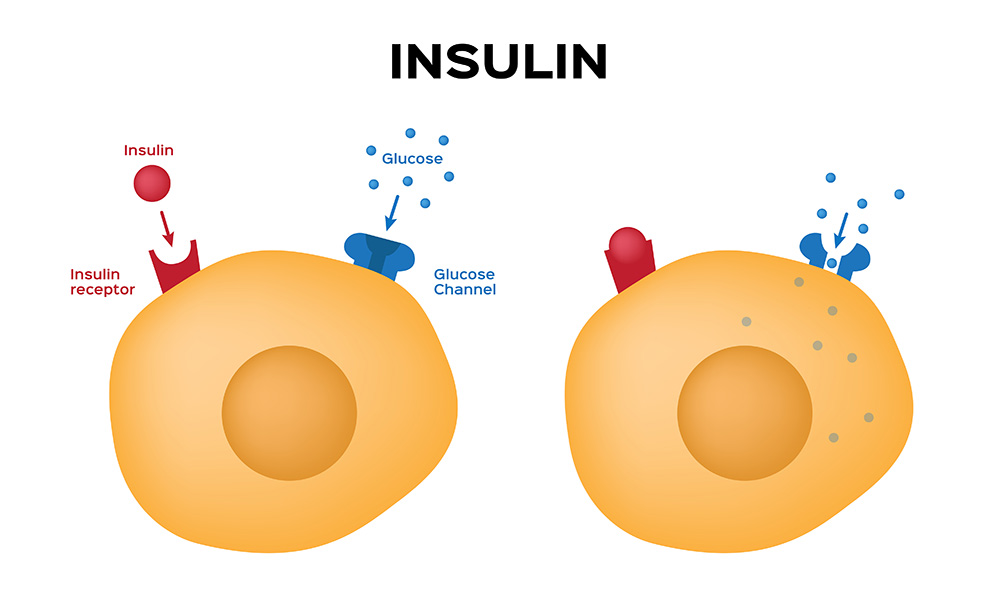
The underlying issue in pre-diabetes is insulin resistance. Insulin is the hormone that allows blood sugar (glucose) to enter our cells to be used for energy. But with pre-diabetes, your body progressively loses sensitivity to insulin.
This process begins years before blood sugar reaches diabetic levels.
Initially, beta cells in the pancreas (where insulin is manufactured) produce more and more insulin to try to keep up with insulin resistance. This causes elevated insulin levels (hyperinsulinemia) while blood sugar levels remain normal.
After a while, the insulin production can’t keep up, allowing blood sugar levels to rise, and pushing the person into pre-diabetes. Symptoms may start to appear as glucose levels rise in the bloodstream, when the glucose can’t easily move into the body cells, they are forced to use alternative less efficient metabolic pathways for energy.
Rising glucose levels mean more yet insulin release from the pancreas cells. They increasingly struggle and literally begin wearing out. Over 5-10 years, most patients with untreated pre-diabetes will see their pancreatic beta cells fail completely. This loss stops natural insulin output, transitioning pre-diabetes into full-blown type 2 diabetes.
What are the symptoms of pre-diabetes?
This stage often comes with relatively subtle symptoms including:
Increased thirst and frequent urination – Rising blood sugar acts like a diuretic, pulling fluids from tissues causing dehydration and extra bathroom visits.
Blurred vision – Fluid changes alter the shape of the lenses in your eyes, impacting your focusing ability. Effects are often temporary as sugar levels spike and drop.
Later symptoms include:
Slow healing – Poor circulation and an impact on white blood cells caused by prolonged higher blood sugar inhibit the body’s natural healing process for small cuts and injuries.
Fatigue – Exhaustion, weakness and irritability are common as your cells struggle to access sugar in the bloodstream for energy properly.
Weight loss – The inability to properly utilise sugar for energy leads to weight dropping despite eating standard amounts.
Yeast infections – such as vaginal thrush.
How is pre-diabetes diagnosed?
A normal level of fasting blood glucose (i.e. measured when you’ve fasted overnight) is less than 5.5mmol/L. A level between 5.5-6.9 mmol/L indicates pre-diabetes, and once the level rises above 6.9 mmol/L, it indicates type 2 diabetes.
Glucose levels vary throughout the day, however, and so to get a better long-term look at a person’s glucose metabolism, we use a blood test called HbA1c. This test measures how much of the haemoglobin in our blood cells has become bound with (or ‘glycated’) with glucose. The higher the level of glycated haemoglobin, the more the red blood cells have been exposed to high levels of glucose.
This test gives us a picture of what’s been happening over the past 2-3 months. An HbA1c level of between 42 and 47 mmol/mol indicates pre-diabetes.
Is pre-diabetes reversible?
Yes.
Pre-diabetes is the early progression of insulin resistance and declining pancreatic function. Catching it early provides a chance to reverse course through exercise, diet and modest medication before permanent cellular damage and type 2 diabetes set in.
The goal is to alter your metabolism to break the vicious cycle of hyperinsulinemia combined with prolonged high blood sugar.
Cutting carbs and losing weight (if you need to) is your first line of defence
Since pre-diabetes is characterised by your body’s inability to properly manage carbohydrate intake, the most direct way to take charge is to restrict carbs. Aim for a low-carb meal plan built around healthy proteins, fruits, vegetables and whole grains. People with pre-diabetes who lose even a modest amount of weight, such as 10% of their body weight, can cut their risk of developing full-blown type 2 diabetes by almost 60%.
Move more to stimulate insulin sensitivity
In addition to diet, exercise is crucial for reversing insulin resistance driving pre-diabetes. Aim for 150 minutes of moderate aerobic activity weekly, like walking, swimming or cycling, to help stimulate insulin sensitivity, while also incorporating 2-3 days of strength training to build calorie-burning muscle mass. Even small boosts in physical activity make a difference!
Don’t underestimate the importance of lifestyle adjustments
Stress, poor sleep and smoking are risk factors, but they also exacerbate pre-diabetes. Cortisol and adrenaline hormones released when stressed trigger blood sugar spikes.
Practising mindfulness or meditation has been shown to improve blood sugar control, and it’s essential to get sufficient sleep (between 8-9 hours per night) if you have pre-diabetes.
Stopping smoking will bring huge health benefits all-round.
Get tested
If it’s been a while since you had a health check-up, or if you’re experiencing some of the symptoms described here, book an appointment to see one of our expert GPs, or book a Well Man or Well Woman health screen.
We can spot problems early on and support you in getting back to vibrant health.