PRIVATE ALLERGY TESTING IN ESSEX
Private Allergy Testing in Esssex
Private Allergy Testing At Essex Private Doctors
Private Allergy Testing At Essex Private Doctors
Around 1 in 4 people in the UK will be affected by an allergy at some point in their lives. If you’ve been experiencing allergic symptoms, allergy testing can be very helpful in identifying the ‘allergen’, or trigger.
We offer Private Allergy Consultations, Skin Prick Allergy Testing, and RAST Testing for both children and adults.

What is allergy?
Allergy is when the body’s immune system erroneously overreacts, producing antibodies and an inflammatory response to something that’s a harmless substance, like pollen.
How a person comes into contact with a particular allergen will often determine the kind of allergic symptom the person may experience. For example. If you inhale tree pollen, or grass pollen, you might experience nasal or respiratory symptoms (e.g. allergic rhinitis- aka hay fever). If you are allergic to shellfish and were to eat prawns, you might experience diarrhoea or stomach pain.
It is possible for any allergen, however, to produce a constellation of symptoms, and some allergic responses can be very severe, causing anaphylaxis. This is a rare condition, which can be life-threatening, and may come on very quickly. It can cause tongue and throat swelling, difficulty breathing, feeling very faint and unwell, and sometimes an itchy, bumpy rash.
Skin Prick Allergy Testing
If you’ve ever found yourself wondering, “Am I allergic to something?”—you’re not alone. Many people suffer from symptoms like hives, lip tingling, unexplained rashes, or year-round hay fever without ever getting a clear answer. That’s where skin prick allergy testing comes in. It’s quick, highly informative, and far less daunting than you might think.
At Essex Private Doctors, we now offer private skin prick allergy testing in Essex—suitable for adults and children alike.
What Is a Skin Prick Test and How Does It Work?
Skin prick testing is one of the most widely used methods for diagnosing IgE-mediated allergies. It’s simple, low-risk, and gives you same-day results.
Here’s how it works:
- Tiny droplets of different allergens (such as tree pollen, house dust mites, nuts, or animal dander) are placed on the surface of your forearm.
- A sterile lancet is used to make a small, shallow scratch through each droplet—just enough to let the allergen touch the immune cells in your skin.
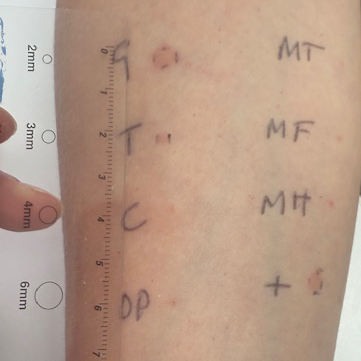
- After around 15 minutes, we check for any visible reactions, like a small red bump (called a “wheal”) which may indicate an allergy.
- We compare each result against a positive and negative control, so you can be confident in what we’re seeing.
The sensation is more like a soft tap or tickle—far more comfortable than a blood test, especially for little ones.

What Allergies Can Be Tested For?
We stock a panel of the 20 most common allergens used in UK allergy testing, including:
- Grass and tree pollen (e.g. birch, oak, ash)
- House dust mite
- Animal dander (dog, cat, horse)
- Common foods like egg, wheat, milk, peanuts, soy, shellfish, sesame
- Mould spores
And if we don’t have the specific allergen in stock (for example kiwi), we can often either order it in or use a sample you bring with you. For example, to test for pollen food syndrome (aka oral allergy syndrome), you might bring in a piece of fresh fruit, which we can use directly on the skin during testing.
Who Should Consider Skin Prick Testing?
Skin prick testing is ideal if you or your child have:
- Reactions after eating—like itchy lips, hives, or swelling
- Suspected hay fever or seasonal allergy symptoms
- Mouth tingling or lip swelling after fruit or vegetables
- A past anaphylactic reaction that’s never been fully investigated
- Chronic rashes or hives with no clear trigger
- Concerns about allergens like pets, pollen, or dust mites
- Year-round nasal symptoms, possibly linked to indoor allergens
It’s also really useful if you want to get strategic with when to start antihistamines—for example, knowing when birch or grass pollen peaks, so you can start nasal sprays and medications before symptoms take hold.
Skin Prick Allergy Testing for Children
Worried your child might have an allergy?
This is a fantastic starting point. Skin prick testing is child-friendly, quick, and can help you avoid unnecessary food restrictions. It’s a better-tolerated alternative to blood testing for many children.
We can test children aged 12 months and upwards, (and sometimes even infants if there’s a clear allergy problem that needs investigating- at the discretion of Dr Eleanor Beddoe).
We’ll gently support your child through the test, and you’ll have results in under 30 minutes. For many parents, it’s a huge relief to finally have answers.
Although IgE blood tests are also available, skin prick testing is often preferred as a first-line investigation because:
- It gives instant results
- It’s better tolerated in young children
Is It Safe?
Yes—very safe. Although there is a theoretical risk of reaction, it’s extremely rare, and we’re fully equipped to deal with any issues. Most people simply experience mild itchiness or redness, which settles quickly.
We never perform skin prick testing without a detailed clinical assessment first. You’ll also stay in the room with us for the entire time, so we can monitor your reaction and discuss results straight away.


Skin Prick Allergy Testing Process
The first step is to book an Allergy Testing Consultation with Dr Eleanor Beddoe, our Allergy Specialist GP. This is important to ensure the right testing for you. It can be an in-person or video consultation.
Some people believe they may be allergic to certain foods, when in fact their symptoms may be intolerance symptoms, as opposed to a true allergy symptoms.
If it’s deemed that skin prick allergy testing is the right next step, you’ll attend for a testing appointment. See our Fees page for more details.
During the test, a drop of a range of different types of allergen are placed onto the skin (usually the inner forearm) and a very fine lancet is used to lightly prick the skin surface, so the allergen gets into the skin’s surface. Next we wait for 15-20 minutes, and the see if there is a positive reaction to a particular allergen (because a ‘weal’ or raised swelling occurs) or if there is a negative reaction (no significant weal). We measure the sizes of the weals to get an indication of the extent of the allergic reaction.
What Happens Next?
If your results confirm an allergy, we’ll explain what that means for your day-to-day life—whether that’s adjusting your diet, making changes at home to reduce dust or pet exposure, or knowing when to start allergy meds in pollen season. If needed, we can:
- Prescribe adrenaline auto-injectors (like EpiPens)
- Write you a clear allergy management plan
- Arrange follow-up testing or referrals
- Help you trial foods again in a safe, supervised way—if your test is negative but your symptoms remain suspicious
If skin testing doesn’t give us a clear answer—or if the medical history points to a more complex picture—we may follow up with blood testing (RAST testing) or refer you to a specialist allergy centre such as Imperial Hospital.
RAST and ALEX² Allergy Blood Tests
At Essex Private Doctors we can help you to determine what’s causing your allergic response, and help you to manage your symptoms, or even avoid the triggering allergen altogether.
RAST stands for radioallergosorbent test; it was the original blood test for investigating allergies, and whilst it’s been replaced with newer tests, we still tend to refer to allergy tests as ‘RAST tests’.
RAST testing involves measuring the levels of antibodies we may produce against different allergens, and the test looks for IgE antibodies, which are the type of antibodies associated with an allergic reaction.
The ALEX² Allergy Explorer Blood Test is a cutting-edge blood test that can screen for up to 300 different allergens from a single blood sample.
This test can detect reactions to a wide range of common allergens, including pollen from trees, grasses, and weeds, as well as house dust mites, cat and dog fur, moulds, yeasts, insect stings, various foods such as nuts, dairy, and eggs, and even latex. It also measures your total IgE level, which helps build a more complete understanding of your immune response.
We may recommend RAST or ALEX² testing as a additional test to complement skin prick allergy testing.

“I went to see Eleanor for a skin prick allergy test, and I have to say—it was a really gentle and reassuring experience.
She started by marking out my skin carefully, so she knew exactly where to place the droplets. Then she applied the test solutions and used a small lancet to lightly prick the skin. It didn’t hurt at all—just a light touch.We waited 20 minutes, and although it got quite itchy where I reacted, it was absolutely manageable. Afterwards, she wrote me a lovely, clear report. I took an antihistamine, and the itchiness settled within half an hour. What I really appreciated was knowing exactly what I was allergic to—it was such a relief to finally have clarity.”…. Sally.
Allergic Rhinitis (Hay Fever)
Allergic Rhinitis can be a distressing condition, and can cause a runny nose (rhinorrhoea), sneezing, itchy eyes and throat, eye redness and watering, coughing, and a feeling of being ‘bunged up’. It’s not always caused by grass or trees (i.e. not all allergic rhinitis is ‘hay fever’), and sometimes people can become sensitised to things around them in their work environment, such as wood dust, animal dander, and dust from grains.
In our clinic, we frequently meet patients who are allergic to the pollen from Birch trees. They will tend to experience symptoms around March to April time, and they may also experience some cross-reaction with pollen from Alder and Hazel trees.
Allergic rhinitis has strong associations with asthma, and allergy testing can be very helpful in identifying the culprit behind the allergic response. Tree pollen can be highly allergenic, and because it’s very fine, it can be carried a long way by the wind. This means you could live a considerable distance from the offending trees, and the cause might only come to light with allergy testing.
Allergic rhinitis isn’t a minor inconvenience. Treating it effectively can help improve your asthma symptoms if you’re a sufferer and help prevent the onset of asthma in children.
Allergic Rhinitis (Hay Fever)

Allergic Rhinitis can be a distressing condition, and can cause a runny nose (rhinorrhoea), sneezing, itchy eyes and throat, eye redness and watering, coughing, and a feeling of being ‘bunged up’. It’s not always caused by grass or trees (i.e. not all allergic rhinitis is ‘hay fever’), and sometimes people can become sensitised to things around them in their work environment, such as wood dust, animal dander, and dust from grains.
In our clinic, we frequently meet patients who are allergic to the pollen from Birch trees. They will tend to experience symptoms around March to April time, and they may also experience some cross-reaction with pollen from Alder and Hazel trees.
Allergic rhinitis has strong associations with asthma, and allergy testing can be very helpful in identifying the culprit behind the allergic response. Tree pollen can be highly allergenic, and because it’s very fine, it can be carried a long way by the wind. This means you could live a considerable distance from the offending trees, and the cause might only come to light with allergy testing.
Allergic rhinitis isn’t a minor inconvenience. Treating it effectively can help improve your asthma symptoms if you’re a sufferer and help prevent the onset of asthma in children.

How is allergic rhinitis treated?
If you’re suffering from allergic rhinitis or hay fever, there are several effective treatments:
If you’re still struggling, book an appointment for an allergy consultation.
Food Allergies
Most food allergic responses are thankfully mild, but some can be very serious. Food allergy triggers an immunological response, whilst food intolerance isn’t caused by your immune system overreacting to certain foods.
Food allergy can cause rashes, swelling of the lips and tongue, sneezing, vomiting, diarrhoea, and tummy pain. You might experience symptoms immediately, or symptoms even days later. Peanuts, milk, eggs, fish, shellfish, wheat, and soya are common allergens, and allergy blood testing (RAST testing), can be very helpful in identifying what’s making you unwell.

Cow’s Milk Protein Allergy
We regularly see babies and young children who have cow’s milk protein allergy (aka cow’s milk protein intolerance), and it can be a real struggle for parents.
There are two types of cow’s milk allergy:
Extensively hydrolysed milk formulas (which have been processed to break down cow’s milk proteins) can be very helpful for infants who are suffering from cow’s milk protein allergy, and at Essex Private Doctors, we can thoroughly assess your baby, and make a treatment plan together.
If you or your child is an allergy sufferer, and you’re looking for help, book a consultation with Dr Eleanor Beddoe. She will take you through a thorough allergy consultation, and organise the appropriate testing and treatment planning.