Let’s talk about something that could be going on in your body right now—without causing a single symptom.
Osteoporosis is one of the most common and overlooked health conditions in the UK, and yet many people only find out they have it after a bone has already broken. That’s because osteoporosis doesn’t cause pain. It doesn’t give you warning signs. It just quietly thins your bones—until one day, you trip on the stairs or bend down to pick 1 something up, and crack.
It’s known as “the silent thief” for a reason.
So what exactly is osteoporosis? Who gets it? How do we test for it? And most importantly, what can you do to prevent it or stop it in its tracks?
Let’s dive in.
What Is Osteoporosis?
Osteoporosis is a condition where your bones become progressively thinner, weaker, and more fragile over time. It happens when the balance between two key types of bone cells—osteoblasts (which build bone) and osteoclasts (which break bone down)—gets thrown out of sync.
Normally, these two types of cells are in harmony, constantly renewing and maintaining your bone strength. But in osteoporosis, the osteoclasts take the lead, breaking down bone faster than the osteoblasts can rebuild it.
At first, this just causes mild bone thinning—what we call osteopenia. But as the process worsens, you end up with full-blown osteoporosis, and that’s when things become dangerous.
Is osteoporosis hereditary?
Yes, genetics can play a role. If one of your parents or siblings has been diagnosed with osteoporosis or has suffered a hip fracture, your risk is significantly higher. In fact, a parental history of hip fracture is included as a major risk factor in tools like the FRAX® score, which we use to assess fracture risk.
But remember—just because it runs in your family doesn’t mean you’re destined to get it. Lifestyle, hormone levels, and diet all play a role too. The key is knowing your personal risk early and taking steps to reduce it.
What causes osteoporosis?
Osteoporosis isn’t caused by just one thing—it usually results from a combination of hormonal changes, lifestyle habits, and medical conditions.
Here are some of the most common causes:
- Hormonal changes – The big one is the drop in oestrogen during menopause (for women) and falling testosterone levels in ageing men.
- Steroid medications – Long-term use of corticosteroids (like prednisolone) can reduce bone formation.
- Chronic illnesses – Conditions like coeliac disease, rheumatoid arthritis, inflammatory bowel disease and some cancers increase risk.
- Poor nutrition or low weight – Not getting enough calcium or vitamin D, or having a very low BMI (such as in eating disorders), can weaken bone.
- Smoking and excess alcohol – Both directly harm bone cells and slow healing.
- Lack of physical activity – Your bones respond to pressure and movement. The less you move, the less stimulus they get to stay strong.
Sometimes it’s a combination of subtle risk factors that build up over time—another reason why proactive screening is so important.
Can osteoporosis be cured?
Here’s the honest answer: osteoporosis can’t be cured in the traditional sense, but it can absolutely be treated—and even reversed to a degree.
The aim of treatment is to:
- Stop or slow further bone loss
- Build new bone (in some cases)
- Reduce your risk of fractures
With the right plan—including medication, lifestyle changes, and hormone support where appropriate—we can dramatically reduce your risk of breaks and help you stay active, mobile and independent.
And the earlier we catch it, the more we can do.
The Real Impact of Fractures: It’s About More Than Just a Broken Bone
Let’s be very clear—osteoporosis isn’t just about bones thinning quietly in the background. The real danger lies in the life-changing consequences that can follow a fracture.
Too often, we think of broken bones as just a temporary inconvenience. A few weeks in a cast, some physiotherapy, and you’re good to go—right?
Sadly, that’s not always the case, especially as we get older.
Hip fractures in particular can be catastrophic.
In fact, in the UK, around 10% of people with a hip fracture die within the first month, and roughly one in three won’t survive beyond a year. That’s not because of the fracture itself, but because of the chain reaction it sets off—immobility, infections, surgery risks, and worsening of other medical conditions.
And for those who do survive, the recovery is often far from straightforward:
- Around 40% are left unable to walk independently
- More than 60% need help with daily tasks like dressing or climbing stairs
- One in three people will need long-term care or a nursing home within a year of the fracture
- 80% say they can no longer manage activities they once took for granted—like shopping, driving, or getting out to see friends
Then there’s the emotional toll. Many patients experience a sharp decline in quality of life, with increased risk of depression, anxiety, and loneliness. It’s not just about broken bones—it’s about losing independence, confidence, and connection.
And let’s not forget the impact on families. The sudden need for round-the-clock care, home adaptations, or financial support can put huge strain on spouses, children, and carers.
Most people don’t know they have osteoporosis until something breaks.
There are no early warning signs. No pain. No dramatic symptoms. You can’t feel your bones getting thinner.
Which is exactly why screening is so important—especially if you’re over 50, postmenopausal, or have risk factors.
When Do Bones Start Thinning?
Our bone density gradually increases from childhood and peaks around age 30. After that, we naturally begin to lose a little bone each year. For women, this loss becomes far more rapid around the time of menopause due to the sharp drop in oestrogen levels—a hormone that plays a crucial role in maintaining bone strength.
In men, bone loss tends to happen more gradually due to the slow decline of testosterone, but some men do go on to develop osteoporosis—particularly if they have certain medical conditions or low testosterone levels.
Risk Factors: Are You at Risk?
You might be surprised to learn that osteoporosis isn’t just about “being old.” There are many lifestyle, medical, and genetic factors that can increase your risk—some of which are very common.
Let’s break them down:
✅ Female, particularly postmenopausal
The drop in oestrogen around menopause is one of the biggest drivers of bone loss. If your menopause came early (before age 45), or you had a hysterectomy without HRT, your risk increases even more.
✅ Family history of osteoporosis
If one of your parents fractured a hip, that’s a big red flag.
✅ Low body weight or history of eating disorders
Being underweight or having had anorexia puts your bones at a disadvantage from the start.
✅ Smoking and excessive alcohol
Both affect bone metabolism and calcium balance.
✅ Medical conditions like:
Rheumatoid arthritis
Coeliac disease
Cancers (e.g., breast cancer, prostate cancer)
Endocrine conditions like hyperthyroidism or low testosterone
✅ Long-term use of certain medications:
Steroids (e.g., prednisolone)
Anti-oestrogen medications (e.g., used in breast cancer)
Anti-epileptic drugs
How to prevent osteoporosis
The good news? Osteoporosis is not inevitable—and there’s a lot you can do to keep your bones strong at every stage of life.
Here’s how to get ahead of it:
- Build a solid foundation early: In your 20s and 30s, weight-bearing exercise (like walking, running, and resistance/weight training) and a calcium-rich diet help you hit your peak bone mass.
- Protect your bones during menopause and beyond: If you’re a woman in your 40s or 50s, this is a critical window. HRT, where appropriate, can protect against bone loss. So can resistance training, vitamin D supplements, and cutting back on smoking and alcohol.
- Stay active as you age: It’s never too late to make a difference. Even light exercise, like brisk walking or balance-based activities (e.g. tai chi), can reduce fall risk and stimulate bone-building cells.
How Do We Assess Your Risk?
At Essex Private Doctors, we don’t wait until you’ve broken something to assess your bone health.
🧮 We start with the FRAX® Score
This is a world-class risk calculator that uses your age, sex, weight, height, lifestyle, and medical history (including things like parental hip fractures or steroid use) to estimate your 10-year risk of a fracture.
You don’t even need a scan to get started—FRAX can give us an excellent idea of whether you’re at low, moderate, or high risk. And if your FRAX score raises concern, we’ll recommend a more detailed assessment.
💡 The DEXA Scan: Our Gold Standard for Diagnosing Osteoporosis
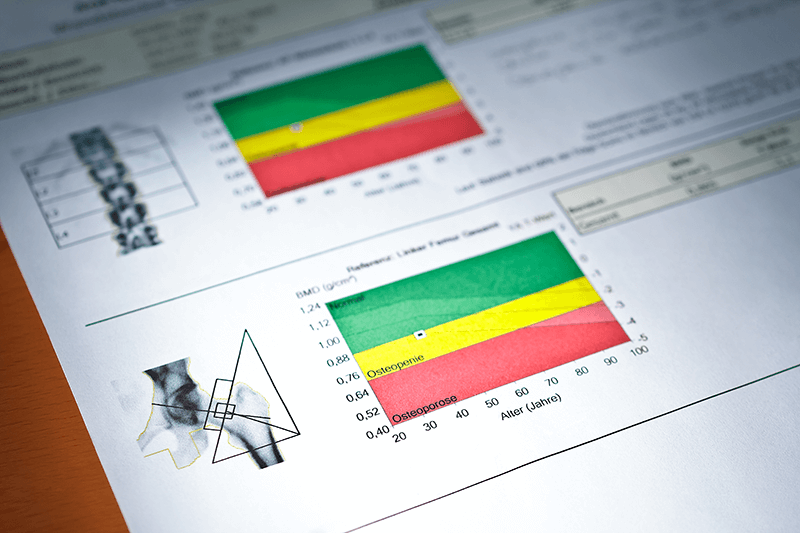
A DEXA scan (short for Dual-Energy X-ray Absorptiometry) is a quick, painless, and highly accurate test that measures your bone mineral density. It’s the gold standard for diagnosing osteoporosis and assessing your risk of fractures. It’s also known as a bone mineral density scan.
During the scan, you’ll lie flat on a padded table while a low-dose X-ray machine passes over your body. It typically takes no more than 15–20 minutes, and you stay fully clothed (you may just need to remove items with metal fastenings).
DEXA scans focus on the spine and hips—the two most common sites of osteoporotic fractures. These areas also give us the clearest picture of your bone strength and fracture risk. Occasionally, other areas like the wrist or forearm may be scanned, particularly if you’ve had previous fractures or can’t have the standard scan.
It’s a completely non-invasive procedure, with less radiation than a dental X-ray, and the results help us decide whether lifestyle changes, supplements, or medication are needed to keep your bones strong.
Understanding T-scores, Z-scores, and the difference between osteopenia and osteoporosis
When you have a DEXA scan, the results come in the form of a T-score and a Z-score—but what do these actually mean?
Your T-score compares your bone density to that of a healthy 30-year-old (when bone mass is at its peak). It tells us how far above or below that benchmark your bone density sits. A T-score between -1.0 and -2.4 means your bones are thinner than average, but not dangerously so—this is known as osteopenia. It’s a warning sign that you’re on the path to osteoporosis, but with the right interventions, you can often slow—or even reverse—this process.
A T-score of -2.5 or lower is the diagnostic threshold for osteoporosis, meaning your bones are fragile enough to be at significant risk of fractures.
Your Z-score, on the other hand, compares your bone density to someone of your own age, sex, and size. While it’s less commonly used for diagnosis in older adults, it can be useful in identifying secondary causes of bone loss—especially in younger patients.
Understanding these scores helps us make better decisions about your treatment, and track how well your bones respond over time.
Signs of Osteoporosis
Remember, osteoporosis doesn’t usually cause symptoms. But once your bones are fragile enough, it can start to show itself in subtle ways, such as:
- Height loss
- Stooped posture (from vertebral fractures)
- Back pain
- Fractures from minor bumps or falls
If these are happening, your bones are already at risk.
What Can You Do About It?
🔸 1. Calcium and Vitamin D
You need enough calcium to build and maintain bone. The International Osteoporosis Foundation has a brilliant calcium calculator where you can check if you’re getting enough from your diet. (Hint: many people aren’t.)
Most adults should aim for 1,000–1,200 mg of calcium per day, plus a vitamin D supplement, particularly in the darker months when sun exposure is low.
🔸 2. Weight-Bearing Exercise
Walking, running, dancing, and resistance training all stimulate bone cells and improve density. We’ll talk you through what’s safe and effective for your fitness level.
🔸 3. Avoid Smoking and Limit Alcohol
These both directly damage bone-forming cells. Even reducing your intake can make a big difference.
🔸 4. HRT (for women)
Hormone Replacement Therapy is one of the most effective treatments to prevent and treat osteoporosis in postmenopausal women, particularly if started within 10 years of menopause. It protects bone density and has a host of other benefits—especially when personalised properly.
🔸 5. Bisphosphonates
These are first-line medications for many people diagnosed with osteoporosis. They reduce the breakdown of bone and lower fracture risk by up to 50%. Options include:
- Oral tablets (e.g., alendronate, taken weekly)
- Yearly infusions (e.g., zoledronic acid)
🔸 6. Denosumab
This is a six-monthly injection that reduces bone breakdown and is particularly good for people who can’t tolerate bisphosphonates.
The Link Between Bone Health and Hormones (Yes, Even in Men)
We often associate osteoporosis with women, but men aren’t immune. Testosterone plays a key role in maintaining bone density—and men with low testosterone are at higher risk of developing osteoporosis. If you’ve noticed signs of fatigue, mood changes, or difficulty building muscle, it may be worth testing your hormone levels too.
Why Screening Is So Important
Osteoporosis is treatable—but it has to be caught early.
A routine DEXA scan can:
- Detect bone loss before a fracture happens
- Guide you toward lifestyle changes that preserve bone health
- Help us start medication if needed to prevent future injury
And just like we check blood pressure and cholesterol in your 40s and 50s, we should be checking bone health too.
How We Can Help
At Essex Private Doctors, we offer:
✅ FRAX score calculations during your consultation
✅ DEXA referral
✅ Personalised bone health plans
✅ HRT and testosterone support if needed
✅ Lifestyle guidance, dietary support, and medication options
You don’t need to wait until you’ve broken a hip or crunched your spine before we step in. Let’s check your risk now, while there’s time to act.